*Researchers at Newcastle University have led a new study that has identified a novel genetic reason for immunological illnesses that are uncommon in children, which could lead to early detection and treatment*
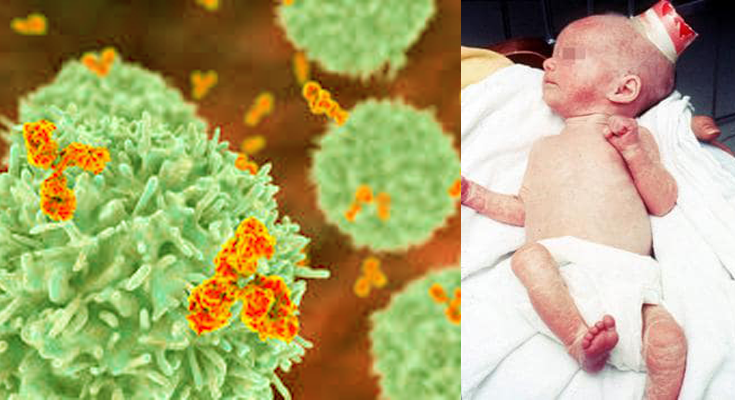
JNS: A form of primary immune deficiency known as severe combined immunodeficiency affects lymphocytes, a type of white blood cell that helps the body fight infections and is particularly important for immunological memory. Because they don’t produce enough T cells, children with SCID are unable to fight off bacterial, viral, and occasionally fungal infections. Despite frequently seeming healthy at birth, infants with SCID can exhibit the disorder’s symptoms—such as bacterial infections, repeated respiratory infections, and failure to thrive—quite rapidly.
A closely related condition known as Omenn Syndrome results from the development of an extremely low number of T lymphocytes—not enough to effectively defend against infection, but enough to produce additional inflammatory issues like skin redness (erythroderma), peeling (desquamation), hair loss (alopecia), and spleen and liver swelling. These illnesses are lethal in infancy if prompt treatment is not received, such as stem cell transplantation to replace the compromised immune system. For this reason, several nations are testing newborns for severe T cell depletion.
The study, which was published in Science Immunology, involved specialists from Newcastle University, the Great North Children’s Hospital in Newcastle, the Wellcome Sanger Institute, and its partners in the Netherlands, Norway, and the United Kingdom. Eleven children from four distinct families were evaluated by the team; two of the children had SCID and the other nine had Omenn syndrome. The 11 children were all discovered to have hereditary mutations that interfered with the NUDCD3 protein’s ability to function. The T and B cells required to fight various infections were unable to mature normally as a result of these abnormalities.
The researchers demonstrated that NUDCD3 mutations impede a crucial gene-rearranging mechanism known as V(D)J recombination through in-depth analyses of patient-derived cells and mice models. The production of the many T cell receptors and antibodies required to identify and combat various infections depends on this mechanism. They discovered that, in contrast to mice created with the same NUDCD3 mutations, who had less severe immunological issues, human patients faced serious, perhaps fatal repercussions. The fact that two individuals recovered following stem cell transplantation highlights how crucial early detection and treatment are.
The lead author of the study, Professor Sophie Hambleton from Newcastle University, is pleased with the outcomes. She is also employed as a paediatric immunologist at the Great North Children’s Hospital. Devastating conditions like SCID and Omenn syndrome necessitate intricate and prompt medical interventions, according to Hambleton, “We can better care for impacted babies if we have a deeper understanding of its underlying causes. While we continue to learn more about how the immune system functions in both health and disease, our research aims to fill in the gaps so that families can obtain a molecular diagnosis.”
One of the study’s authors, Dr. Gosia Trynka, stated that early diagnosis can mean the difference between life and death for newborns with high-risk immunodeficiencies. These illnesses render babies virtually defenceless against infections that the majority of us can resist. The discovery of this novel illness gene will enable medical professionals to diagnose afflicted people with a new disease more rapidly and provide them with life-saving therapies.
The results of this study pave the way for early SCID and OS diagnosis, intervention, and genetic counselling for impacted families. While T cell deficiency can be identified by newborn screening techniques, understanding the precise genetic aetiology of SCID boosts diagnostic confidence and influences the selection of a curative treatment. But for at least one in ten families impacted by SCID and OS, this is still out of reach.